Opioid Settlement
Opioid Settlement
Buncombe County is set to receive $16 million over a period of 18 years through the Opioid Litigation Settlement. Communities can use these dollars to help attain outcomes for residents through treatment, recovery, harm reduction, and other life-saving programs and services. Pharmaceutical companies have also agreed to certain steps that limit the distribution and sale of opioids. For more information, including North Carolina's opioid settlement dashboard, go to https://ncopioidsettlement.org.
Frequently Asked Questions
According to the Memorandum Of Agreement
Between The State of North Carolina and Local Governments on Proceeds Relating to the Settlement of Opioid Litigation, Option A outlines the following as approved strategies for the use of Opioid funds.
1. Collaborative strategic planning. Support collaborative strategic planning to address opioid misuse, addiction, overdose, or related issues, including staff support, facilitation services, or any activity or combination of activities listed in Exhibit C to the MOA (collaborative strategic planning).
2. Evidence-based addiction treatment. Support evidence-based addiction treatment consistent with the American Society of Addiction Medicine’s national practice guidelines for the treatment of opioid use disorder – including Medication-Assisted Treatment (MAT) with any medication approved for this purpose by the U.S. Food and Drug Administration – through Opioid Treatment Programs, qualified providers of Office-Based Opioid Treatment, Federally Qualified Health Centers, treatment offered in conjunction with justice system programs, or other community-based programs offering evidence-based addiction treatment. This may include capital expenditures for facilities that offer evidence-based treatment for OUD. (If only a portion of a facility offers such treatment, then only that portion qualifies for funding, on a pro rata basis.)
3. Recovery support services. Fund evidence-based recovery support services, including peer support specialists or care navigators based in local health departments, social service offices, detention facilities, community-based organizations, or other settings that support people in treatment or recovery, or people who use drugs, in accessing addiction treatment, recovery support, harm reduction services, primary healthcare, or other services or supports they need to improve their health or well-being.
4. Recovery housing support. Fund programs offering recovery housing support to people in treatment or recovery, or people who use drugs, such as assistance with rent, move-in deposits, or utilities; or fund recovery housing programs that provide housing to individuals receiving Medication-Assisted Treatment for opioid use disorder.
5. Employment-related services. Fund programs offering employment support services to people in treatment or recovery, or people who use drugs, such as job training, job skills, job placement, interview coaching, resume review, professional attire, relevant courses at community colleges or vocational schools, transportation services or transportation vouchers to facilitate any of these activities, or similar services or supports.
6. Early intervention. Fund programs, services, or training to encourage early identification and intervention for children or adolescents who may be struggling with problematic use of drugs or mental health conditions, including Youth Mental Health First Aid, peer-based programs, or similar approaches. Training programs may target parents, family members, caregivers, teachers, school staff, peers, neighbors, health or human services professionals, or others in contact with children or adolescents.
7. Naloxone distribution. Support programs or organizations that distribute naloxone to persons at risk of overdose or their social networks, such as Syringe Service Programs, post-overdose response teams, programs that provide naloxone to persons upon release from jail or prison, emergency medical service providers or hospital emergency departments that provide naloxone to persons at risk of overdose, or community-based organizations that provide services to people who use drugs. Programs or organizations involved in community distribution of naloxone may, in addition, provide naloxone to first responders.
8. Post-overdose response team. Support post-overdose response teams that connect persons who have experienced non-fatal drug overdoses to addiction treatment, recovery support, harm reduction services, primary healthcare, or other services or supports they need to improve their health or well-being.
9. Syringe Service Program. Support Syringe Service Programs operated by any governmental or nongovernmental organization authorized by section 90-113.27 of the North Carolina General Statutes that provide syringes, naloxone, or other harm reduction supplies; that dispose of used syringes; that connect clients to prevention, treatment, recovery support, behavioral healthcare, primary healthcare, or other services or supports they need; or that provide any of these services or supports.
10. Criminal justice diversion programs. Support pre-arrest or post-arrest diversion programs, or pre-trial service programs, that connect individuals involved or at risk of becoming involved in the criminal justice system to addiction treatment, recovery support, harm reduction services, primary healthcare, prevention, or other services or supports they need, or that provide any of these services or supports.
11. Addiction treatment for incarcerated persons. Support evidence-based addiction treatment, including Medication-Assisted Treatment with at least one FDA-approved opioid agonist, to persons who are incarcerated in jail or prison.
12. Reentry Programs. Support programs that connect incarcerated persons to addiction treatment, recovery support, harm reduction services, primary healthcare, or other services or supports they need upon release from jail or prison, or that provide any of these services or supports.
Buncombe County runs on a fiscal year, which is July 1st through June 30th.
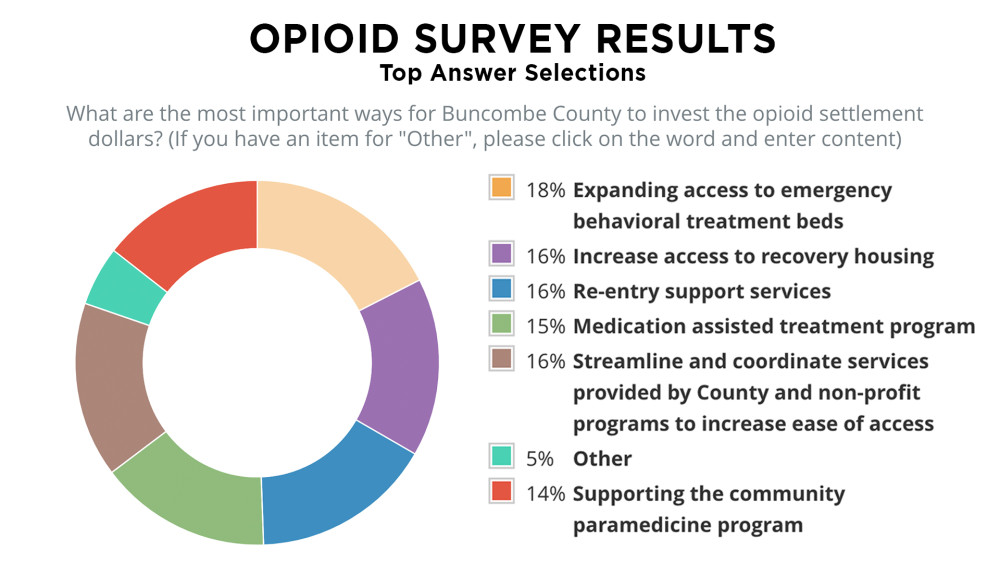
"Other" Responses were: Harm reduction services; Money to increase the length of stay in inpatient treatment; Initiatives targeted to adolescents, even intensive outpatient